June 2025 Newsletter | From Awareness to Action
My mission is to be the first woman in 4 generations to not develop Alzheimer’s Disease (AD). On my journey of discovering ways to mitigate my risk, I pass this information on to you in this Brain-Body-Health (BBH) Newsletter.
Hello Brain-Body-Health Citizen Scientists
Dementia is tricky for our bodies and our brains. Like a curve ball, we can’t see it coming. It’s insidious and sneaky. It hides by attacking our brains at a snails pace. It doesn’t go for the jugular. It starts cutting like an evil editor on things you won’t notice. By the time you wonder if something is wrong with your brain, the damage is taking it’s toll. It’s a conundrum because memory impairment robs us of what just happened—our immediate—short-term memory. This is how it tricked scientists for decades leading to the normalization of memory impairment. It's why my grandmother was diagnosed only when she could not longer care for herself. The thinking back then was: you get old and you get forgetful.
This normalization of cognitive impairment as a typical part of aging has significantly hindered progress in Alzheimer’s research by masking early warning signs and delaying crucial interventions. First, it contributes to delayed diagnosis, as early symptoms are often dismissed rather than investigated, resulting in missed opportunities for timely treatment and participation in clinical trials. This delay feeds into an underestimation of Alzheimer’s prevalence, skewing data and limiting the perceived urgency for research funding and policy support. Additionally, the stigma and denial reinforced by normalization prevent individuals and families from seeking medical help, perpetuating a cycle of silence and inaction. On a systemic level, this mindset has historically led to a reduced focus on research, where scientists and funders overlooked the early, more treatable stages of the disease. Clinical trials have also suffered, as participant recruitment is skewed toward later stages, reducing the chances of therapeutic success. Lastly, the broad acceptance of cognitive decline as inevitable discourages policy and funding support, leaving Alzheimer’s initiatives under-funded.
Thanks to advances that emphasize early detection and proactive care this old narrative around Alzheimer’s is shifting. I spoke about these new developments and HOPE in my July BBH Newsletter titled Dementia Dilemma. New tools like blood-based biomarkers for Amyloid and Tau proteins is a step in this direction. Clinically, Alzheimer’s is now seen as a continuum, with growing recognition of preclinical and prodromal stages—encouraging diagnosis and treatment earlier than ever before. An example of this is the FDA-approved drugs like Lecanemab (Leqembi) that my brother has taken, which work best when administered in the early stages. Public awareness campaigns are also helping reduce stigma and promote early intervention. Although funding instability poses a challenge, recent research and global health initiatives are pushing towards prevention, biomarkers, and personalized care. Together, these changes are replacing outdated assumptions with more hopeful, science-driven, approaches to Alzheimer’s.
Changing the narrative around Alzheimer’s starts with raising awareness and promoting early action. Here’s what you can do:
Educate Yourself and Others:
Know the difference between normal aging and early signs of Alzheimer’s. Share accurate information to help your friends, family, and community recognize when memory issues need attention.
Encourage Early Screening:
Advocate for your own cognitive health by requesting cognitive check-ups, especially if there’s a family history or concerns. Early diagnosis opens the door to more effective treatments and participation in clinical trials.
Support Research and Advocacy Groups:
Get involved with or donate to organizations pushing for better funding, research, and public education on Alzheimer’s.
Help Reduce Stigma:
Speak openly about cognitive health to normalize conversations around memory loss, making it easier for people to seek help without fear or shame.
Promote Healthy Lifestyle Choices:
Encourage habits shown to reduce Alzheimer’s risk, such as regular exercise, a balanced diet, mental stimulation, and social engagement. Refer to SLEDSSSS on my website
Engage with Policymakers:
Support policies that increase funding for Alzheimer’s research, improve healthcare access, and expand support services for patients and caregivers.
The NIH is facing steep proposed budget cuts—dropping from $47 billion to around $27-28 billion. Over 2,000 grants worth up to $12 billion have been canceled or frozen, directly impacting Alzheimer's research.
What can we do?
Due to these cuts, I will be joining my family in September for the Alzheimer’s Association’s Walk to End Alzheimer’s. My cousin Carol, who has Alzheimer’s Disease, will be walking with us, and I’m dedicating my walk to my mother, Gladys Gleason.
Think of life like my mother did. She was the CEO (Chief Entertainment Officer) of the Virginal Experience Club. We read this at her memorial 5 years ago.
Mission Statement
Virginal Experience Club:
Commit to an ongoing search for
new joyful experiences in life
Expanding appreciation
of friendships, talents, laughter and tears
Continue to note the beauty in all
people, nature, feelings, the seen and unseen
Disregard age as an excuse for being child-like,
spontaneous or free
Share the excitement with others
of deepened intuition, awareness, and
discoveries
Maybe you, too, would like to support this research. Together, we can end Alzheimer’s Disease. If you want to donate to our walk, please visit my page.
Lessons from Coaching:
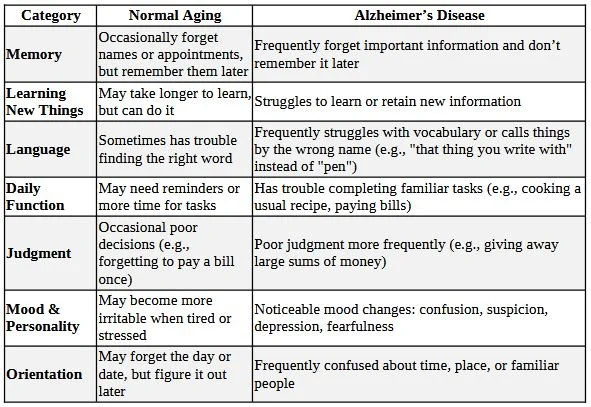
One of the questions I get asked frequently: "What is the difference between normal aging and abnormal aging, i.e., Alzheimer's Disease." Here’s the breakdown:
🧠 Normal Aging vs. Alzheimer’s Disease
🚩 Red Flags Suggestive of Alzheimer’s
Getting lost in familiar places
Repeating questions or stories over and over
Trouble with planning or problem-solving (e.g., following a recipe, managing finances)
Difficulty recognizing familiar faces
Withdrawal from work or social activities
Misplacing things and being unable to retrace steps
Next Steps: If you are concerned about your memory:
Make an appointment with your primary care provider. Make sure you ask if standard cognitive tests are offered like: MoCA (Montreal Cognitive Assessment) or MMSE (Mini-Mental-Status-Exam).
A neurologist or geriatrician can do a full cognitive assessment. I generally refer to the closest University Memory Center.
Laboratory and other tests are listed here on my website.
Brain Body Health is a coaching practice to assess your risk of Alzheimer’s Disease and related dementias. I offer coaching sessions to help navigate and improve brain health for you or a loved one. Contact me to schedule a session or talk to your organization.
Lessons from Science:
🧠 Blood Tests for Alzheimer’s Disease — What’s New?
1. FDA-Cleared Blood Tests for AD Diagnosis
The Lumipulse pTau217/β-amyloid blood test recently became the first FDA-cleared test to detect key Alzheimer's biomarkers in blood samples of adults aged 55 and older.
This test measures phosphorylated tau (pTau217) and amyloid-beta proteins, which are hallmarks of AD pathology in the brain.
It offers ~90% accuracy in predicting AD-related brain changes compared to PET scans or cerebrospinal fluid (CSF) analysis, which are invasive and expensive.
2. Early Detection Potential
Research shows these blood tests can detect Alzheimer’s-related protein changes up to 15–20 years before symptoms appear.
Early detection opens the door to earlier intervention, lifestyle changes, and enrollment in clinical trials for novel treatments.
3. Clinical Utility and Impact
With blood tests, primary care doctors can easily screen patients, leading to faster diagnosis and reducing reliance on specialized imaging or lumbar punctures.
4. Ongoing Research and Improvements
Scientists are continuously refining blood tests to improve sensitivity, specificity, and to differentiate Alzheimer's from other dementias.
In a nutshell:
Blood tests for Alzheimer's Disease are transforming early diagnosis, making screening more practical and less invasive. They hold great promise for improving patient outcomes by enabling timely intervention, but need to be used thoughtfully within a comprehensive clinical framework.
My most recent talk on, “The Dementia Dilemma”, is now available to view.
To optimal health and peace for all!
Subscribe to the email list for news and updates on Body-Brain Health
“If you want to go FAST, go alone. If you want to go FAR, go together."
- African proverb
To our optimized health!